DMARDs (Disease-modifying antirheumatic drugs)
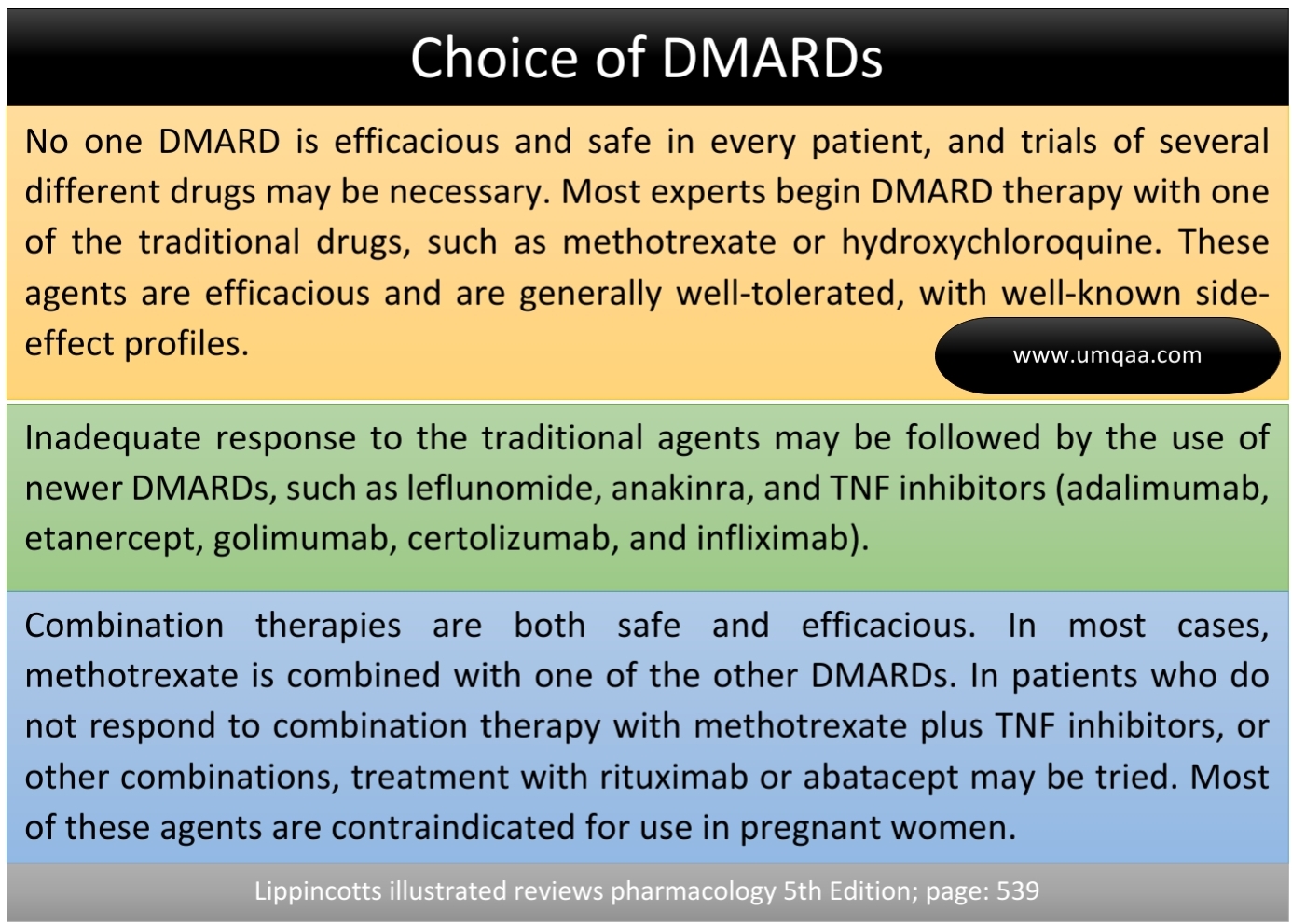
DMARDs are a group of drugs used in inflammatory rheumatic diseases and other chronic inflammatory conditions. They inhibit various small molecules of the immune response system. In the process, almost all of the DMARDs have the potential to cause liver toxicity and bone marrow suppression, hence needing regular monitoring. If toxicity occurs, treatment may need to be stopped temporarily and resumed at a lower dose. If toxicity is severe, therapy may have to be withdrawn completely and substituted with other drugs.
In this post, we are going to see the available DMARDs. It also includes the indications, doses, mechanism of action, adverse effects, and contraindications of most of the drugs.
Methotrexate (MTX)
Indication: Rheumatoid arthritis(RA), Juvenile Idiopathic Arthritis(JIA), psoriatic arthritis(PsA), axial Spondyloarthritis (AxSpA)
Dose: It is given orally in a starting dose of 10–15 mg weekly and escalated in 2.5 mg increments every 2–4 weeks to a maximum of 25 mg weekly until benefit or toxicity occurs.
Mechanism of action: It inhibits folic acid reductase, preventing the formation of tetrahydrofolate, which is necessary for DNA synthesis in leucocytes and other cells.
- Nausea, vomiting, malaise
- Acute pulmonary toxicity (pneumonitis)
- Hepatitis
- Myelosuppression
- Pulmonary fibrosis
- Mucositis
Monitoring:
Adverse effects:
Adverse effects:
Adverse effects:
Adverse effects:
Adverse effects:
Adverse effects:
Adverse effects:
Adverse effects:
Monitoring:
Monitoring:
Monitoring:
- FBC, LFTs
In pregnancy: MTX must be co-prescribed with robust contraception in women of childbearing potential and treatment must be stopped for 3 months in advance of planning a pregnancy.
During Breastfeeding: Contraindication
Sulfasalazine(SSZ)
Indication: RA, JIA, PsA, AxSpA
Dose: The usual starting dose is 500 mg daily, orally, escalating in 500 mg increments every 2 weeks to a maintenance dose of 2–4 g daily until benefit or toxicity occurs.
Mechanism of action: Incompletely understood
- Nausea and gastrointestinal intolerance
- Leucopenia /Myelosuppression
- Abnormal LFTs
- Rashes /hypersensitivity
- Macrocytosis
- FBC, LFTs
In pregnancy: Safe to use.
During Breastfeeding: Can be used.
Extra: Orange staining of urine and contact lenses may occur.
Hydroxychloroquine (HCQ)
Indication: RA, SLE
Dose: 200-400 mg daily, orally
Mechanism of action: Incompletely understood
- Retinopathy
- Keratopathy
- Ciliary body involvement
- Lens opacities (lenticular deposits)
- Vision
In pregnancy: Safe to use.
During Breastfeeding: Safe.
Leflunomide
Indication: RA, JIA, PsA
Dose: 10-20 mg daily orally
Mechanism of action: It works by inhibiting dihydro-orotate dehydrogenase, an enzyme used by activated lymphocytes to synthesize pyrimidines necessary for DNA synthesis.
- Hepatotoxicity
- Hypertension and headache
- Hirsutism
- Rashes
- Weight loss
- Reduce sperm counts
- Marrow toxicity
- Pneumonitis
- FBC, LFTs, BP
In pregnancy: It must be co-prescribed with robust contraception in women of child-bearing potential. Treatment must be stopped for 2 years in advance of planning a pregnancy.
Azathioprine
Indication: Systemic vasculitis (SV), SLE
Dose: Starting dose is 1 mg/kg body weight per day, increasing to 2.5 mg/kg until a response is observed or toxicity occurs
Mechanism of action: It is metabolized to 6-mercaptopurine (6-MP), which blocks lymphocyte proliferation by inhibiting DNA synthesis
- Bone marrow suppression
- Hepatotoxicity
- Pancreatitis
- Nausea and vomiting
- FBC, LFTs
In pregnancy: Safe to use.
During Breastfeeding: not recommended
Extra: Allopurinol inhibits catabolism of azathioprine, necessitating a 75% reduction in azathioprine dose. Genetic polymorphisms in the enzyme thiopurine S-methyltransferase (TPMT) influence the catabolism of 6-MP.
Apremilast
Indication: PsA
Dose: 30 mg twice daily orally
Mechanism of action: It works by inhibiting phosphodiesterase D4 in leucocytes, which in turn suppresses the production of pro-inflammatory cytokines, thereby reducing inflammation.
- Gastrointestinal upset
- Weight loss and
- Increased risk of depression
- Not necessary
Janus-activated kinase (JAK) inhibitors
Available drugs: Tofacitinib & Baricitinib
Indication: RA, an alternative to biologic treatment
Dose: Tofacitinib is given orally in a dose of 5 mg twice daily and Baricitinib is given orally in a dose of 2–4 mg once daily
Mechanism of action: Inhibit JAK(Janus-activated kinase) enzymes, which are a family of intracellular signaling molecules that play a key role in transducing the effects of several proinflammatory cytokines
- Increased risk of opportunistic infections
- Hepatotoxicity and
- Hematological toxicity
- LFTs, CBC, and infection
Cyclophosphamide
Indication: SV, SLE
Dose: It can be given orally in a dose of 2 mg/kg/ day for 3–6 months or intravenously in a dose of 15 mg/kg every 3–4 weeks on 6–8 occasions.
Mechanism of action: Cytotoxic alkylating agent that cross-links DNA and halts cell division, causing immunosuppression.
- Nausea, anorexia, vomiting
- Bone marrow suppression
- Cardiac toxicity
- Alopecia, and
- Hemorrhagic cystitis.
- FBC, LFTs, eGFR
Extra: The risk of cystitis can be mitigated by co-administration of mesna (2-mercaptoethane sulfonate, which binds its urotoxic metabolites) and a high fluid intake.
Mycophenolate mofetil (MMF)
Indication: SLE, SV
Dose: 2–4 g daily orally
Mechanism of action: Inhibit inosine monophosphate dehydrogenase, a rate-limiting enzyme in the synthesis of guanosine nucleotides in lymphocytes.
- Hematological toxicity
- FBC, LFTs
Gold (sodium aurothiomalate, myocrisin)
Indication: RA
Dose: Intramuscular injection of 50 mg weekly after an initial test dose of 10 mg. If effective then gradually reduce the frequency ( two-weekly, then monthly).
Mechanism of action: Unknown
- FBC, urinalysis
Penicillamine
Indication: RA
Dose: Starting dose of 125–250 mg daily on an empty stomach, and increased in 125 mg increments every 6 weeks to a maximum dose of 1500 mg daily until there is a clinical benefit or adverse effects occur.
Monitoring:
- FBC, LFTs, urinalysis
Ciclosporin A
Indication: RA, PsA
Dose: 2.5–4 mg/kg/day orally.
Mechanism of action: Calcineurin inhibitor that inhibits lymphocyte activation.
- BP, eGFR
Additional:
DMARDs during pregnancy and breastfeeding:
- Prednisolone, Sulfasalazine, hydroxychloroquine, and azathioprine are safe during pregnancy
- Prednisolone, hydroxychloroquine, and Sulfasalazine are considered safe during breastfeeding
- Azathioprine, cyclophosphamide, methotrexate, and cyclosporine are contraindicated during breastfeeding
Sources:
- Davidson's Principles and Practice of Medicine 23rd; page- 1004






0 Comments