Behçet’s disease
It is also called Behçet’s syndrome. It is a vasculitis of unknown cause which targets small arteries and venules. It is characterized by recurrent mouth and genital ulcers, ocular lesions, and skin, joint & neurological involvement. It is a recurrent, multifocal disorder that persists over many years.
It is rare in Western Europe but more common in ‘Silk Route’ countries, around the Mediterranean and in Japan. It has a strong association with HLA-B51. Association with B12, DR2, DR7 and Drw52 are also found.
Clinical features of Behçet’s disease
- Oral and genital ulcers: These are present in most of the patients. Oral ulcers are universal; deep and multiple, and last for 10–30 days. Ulcers can affect the pharynx and cause dysphagia. Genital ulcers are found in 60–80% of the patients and can cause dysuria and dyspareunia.
- Eye involvement: Ocular lesions are the most serious development. Recurrent uveitis (anterior and posterior both) and iridocyclitis, retinal vascular lesions and optic atrophy can lead to loss of vision in 50% of patients with ocular involvement
- Skin lesions: The usual skin lesions are erythema nodosum. Other skin manifestations include diffuse pustular rash affecting the face (acneiform lesions), erythema multiforme, features of migratory thrombophlebitis and vasculitis etc
- Joints involvement: Seronegative arthritis (mono or oligo-arthritis) affects about 40% of patients and commonly involves knees, ankles, wrists and elbows
- Vascular involvement: Recurrent thrombophlebitis of the legs is a significant feature of Behçet’s syndrome, leading to venous thrombosis. Less often, superior or inferior caval thrombosis may occur
- GIT involvement: Anorexia, abdominal pain and bloody diarrhoea have also been documented
- Neurological involvement: Neurological complications occur in 20% of patients. Organic confusional states, meningoencephalitis, transient or persistent brainstem syndromes, multiple sclerosis and parkinsonian-type disorders are all recognized
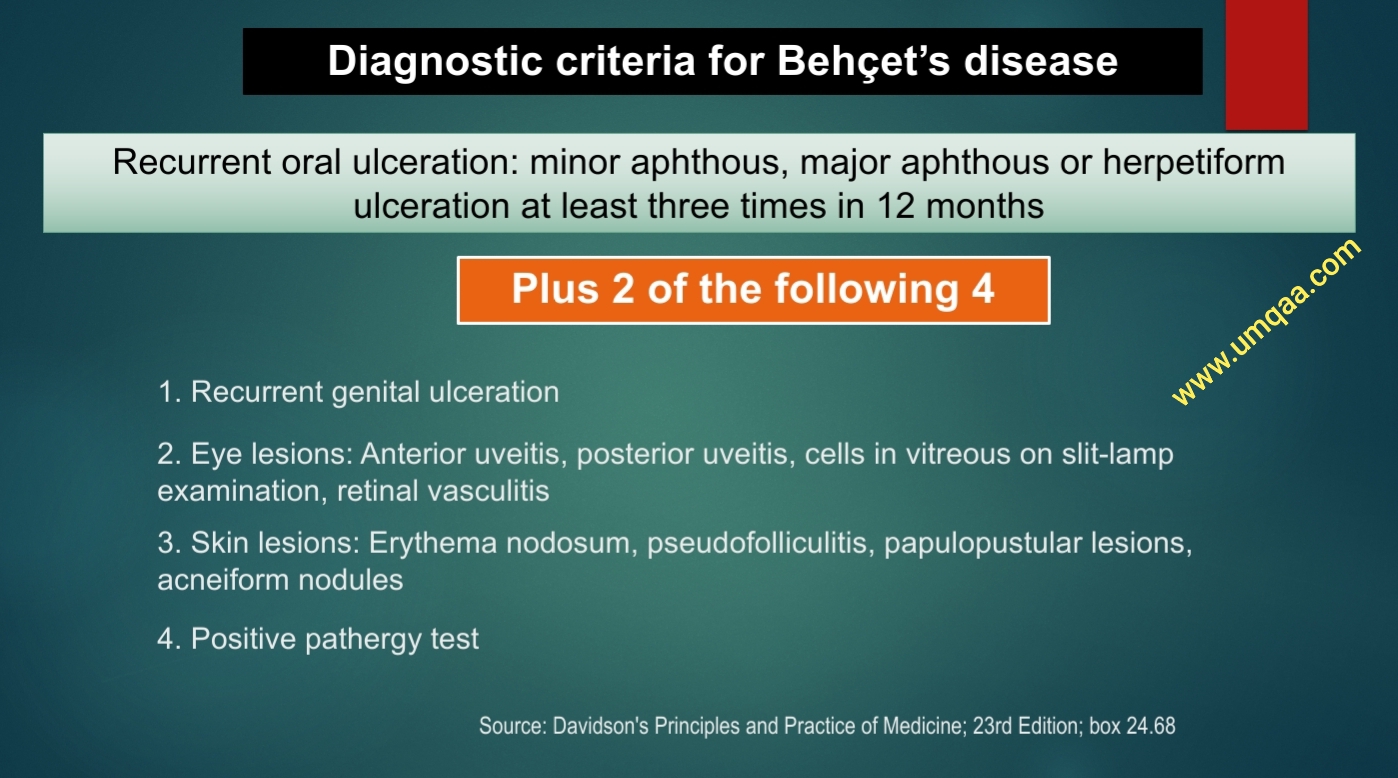
Diagnosis of Behçet’s disease:
- It is a clinical diagnosis. There is no specific diagnostic test except for the pathergy test.
- Pathergy test: It is specific to Behçet’s disease. Pricking the skin with a needle leads to the development of pustular lesion within 24–48 hours.
- ESR and CRP are usually elevated
- Asymptomatic proteinuria is found
Treatment of Behçet’s disease
- Oral ulceration can be managed with topical glucocorticoid preparations (soluble prednisolone mouthwashes, glucocorticoid pastes)
- Colchicine can be effective for erythema nodosum and arthralgia
- Thalidomide (100–300 mg per day for 28 days initially) is very effective for resistant oral and genital ulceration but is teratogenic and neurotoxic
- Glucocorticoids and immunosuppressants are indicated for uveitis and neurological
- Anti-TNF agents can be used to control severe uveitis and serious manifestations such as neurological and gastrointestinal Behçet's disease.
Diagnostic criteria for Behçet’s disease (in the image):
Source:
- Davidson's Principles and Practice of Medicine; 23rd Edition; page 1043
- Kumar and Clark's clinical medicine, 9th Edition; page 702
- Rapid review of clinical medicine for MRCP part 2, 2nd Edition, by Sanjay Sharma and Rashmi Kaushal; Q 31





0 Comments